
Guide osteoarthritis – Wear of the joints
Osteoarthritis is a widespread silent condition which, as it progresses, can substantially degrade the quality of life of afflicted persons due to pain and impairments in day-to-day activities. It is the world’s most common joint ailment in adult population. Approx. 8 million people are suffering from the symptoms of osteoarthritis in Germany alone. That is every 10th inhabitant.
Pain in the joints
What can be done in cases of wear of the joints and cartilage degeneration?
Osteoarthritis · What is that?
Osteoarthritis is the world’s most common joint ailment. Almost everyone knows its effects at some point of life. The number of young people who are affected is also increasing. Osteoarthritis does not form overnight. Joint wear due to cartilage degeneration can develop over years. Often, early stages cause hardly any discomfort, so that the disease is hardly noticed at first.
Many patients report that they feel pain every time they move or stress the arthrotic joints. Pain showing after periods of inactivity or a stiffness of the joints in the morning that improves with repeated movement are characteristic for early stages of osteoarthritis. Persisting pain in resting phases or at night can already be regarded as a symptom of advanced osteoarthritis. Pain may be increased by physical stress or in cold or humid weather. Patients also often describe a creaking in the joints.
Osteoarthritis · Causes
Bones are connected to each other with flexible joints. The contact areas are covered in cartilaginous tissue which prevents the bones from rubbing against each other. The cartilage consists of the chondrocytes and the extracellular matrix (ECM) which is produced by the chondrocytes.
Injuries, improper physical stress (worsened by overweight), disorders in the cartilage metabolism or misregulations in the formation or breakdown of the extracellular matrix can result in cartilage defects.[1] Some antibiotics (gyrase inhibitors) may also further cartilage breakdown. If the chondrocytes can no longer be activated to repair the matrix, the cartilaginous tissue degenerates with osteoarthritis as a consequence.[2]
Stages of osteoarthrits
Early stage · Osteoarthritis grade 1
Usually, osteoarthritis begins with only a small damage to the cartilage. When that expands and first changes on the bone develop (a process that is visible in MRI), it is regarded as osteoarthritis.
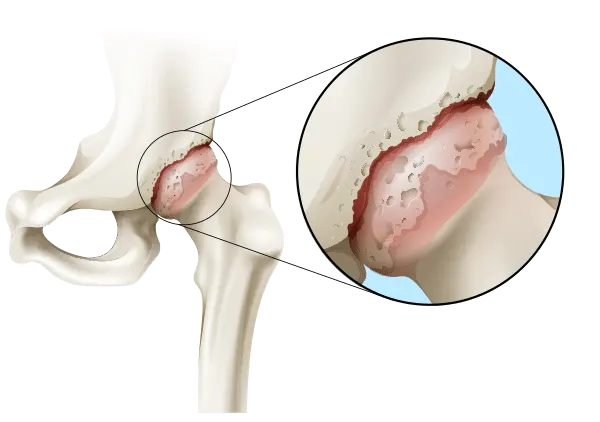
Intermediate stage · Osteoarthritis grade 2 and 3
The joint cartilage loses its flexibility and becomes brittle. The structure of the cartilage cells is damaged. Some bone surfaces are already exposed and rub on each other during movement. This can cause severe pain. Superfluous bone substance can form (subchondral sclerotisation), even subchondral cysts with a diameter of up to one centimetre may develop.
Advanced stage · Osteoarthritis grade 4
Larger bone surfaces without cartilage covering (chondral defects) start to develop. The cartilage wear is so massive that the joint gap is hardly present anymore. By now, the pain often becomes unbearable during movement and often also when resting. This can result in articular effusion (hydrops articularis) with visible and palpable swellings and a restriction of the joint's flexibility. The adjoining muscles, ligaments, tendons and articular capsules may be damaged. Due to these changes to the bones, the joint eventually might even stiffen completely.
Types of osteoarthritis
Osteoarthritis can affect virtually all joints if the cartilage is damaged.
An arthrosis in multile joints at the same time is called polyarthrosis.
Posttraumatic arthrosis is not caused by degeneration but is a consequence of an injury.
Treatment options for osteoarthritis
Many treatments are purely symptomatic and do not stop the arthrotic process but only help with the pain for a while. Injections or intravenous infusions with painkillers, hyaluronic acid and other medication are usually combined with physiotherapeutic measures to relieve the symptoms. However, in these cases the disease itself progresses. In the end, a surgical procedure might become necessary to replace the worn out joint with an artificial one.
Risk joint replacement · Total endoprotheses · TEP
Every year, more than 400,000 artificial knee and hip joints are implanted in Germany alone.[3] Thousands of these require further surgical procedures due to various complications such as infections, thrombosis, embolisms, nerve damage, fractures, calcification or prosthetic loosening. Recent data of a meta study shows that every fifth patient is not content with his knee endoprothesis because of pain, infections, prosthetic loosening or restrictions of movement, among others.[4]
MBST in the treatment of osteoarthritis
Molecular biophysical stimulation
The non-surgical MBST therapy has a different therapy approach and aims at preserving the natural joint. It targets the degeneration of cartilage – one of the major causes for osteoarthritis.
The metabolism is the basis for all vital body processes and requires a lot of energy. This energy is also needed in cartilage tissue to form, preserve and repair the tissue. If the cartilage cells lack energy, endogenous repair mechanisms can no longer be performed and cartilage degeneration occurs. Chondrocytes in the distinct zones of hyaline cartilage differ in size, shape and metabolic activity. Each chondrocyte is responsible for maintaining the extracellular matrix and metabolism in its direct vicinity.[2] Small defects can partly be repaired by healthy chondrocytes. But cartilage tissue contains few blood vessels and has a slow metabolic activity so that regeneration takes a long time. Defects in the articular cartilage affect the repair mechanism due to insufficient matrix metabolism. Then the cartilage cells have to increase their metabolism to keep up the ECM metabolism. In the degenerative arthritic processes, the chondrocytes are no longer able to compensate for the degenerated cartilage. The consequence may be an irreparable and complete loss of the layer of cartilage.[2]
This is the starting point for MBST therapy. The MBST therapy system has been developed to transfer energy to the cartilaginous tissue in a targeted manner. Its objective is to increase the metabolism and thereby re-trigger the body’s own repair mechanisms and regeneration processes. MBST therapy thus directly tackles one of the causes[5] of osteoarthritis.
MBST therapy is based on the physical principle of magnetic resonance, in which hydrogen nuclei take up energy and then release it again partly into the surrounding tissue. Scientific data suggests that MBST magnetic resonance technology stimulates various biophysical processes and triggers anti-inflammatory and pain-relieving effects.[6,7,8] Damaged cells shall be influenced in such a way that natural regenerative processes can be triggered. The treated tissue shall regain as much functionality as possible.
Other indications
MBST magnetic resonance therapy is used not only for osteoarthritis but also for the treatment of other damages to cartilage tissue, i. e. meniscal lesions. Please consult a doctor in an MBST treatment centre to find out if your complaints can be treated as well with MBST magnetic resonance therapy.
The advantages of MBST magnetic resonance therapy in cases of osteoarthritis at a glance:
[1] Buckwalter et al. 2005, Articular Cartilage and Osteoarthritis, Instr Course Lect 54, 465–480 · [2] Martinek et al. 2003, Deutsche Zeitschrift für Sportmedizin, 54/6 · [3] RKI und DESTATIS 2015, Häufigste Operationen in Deutschland · [4] https://www.aerzteblatt.de/nachrichten/83545/Jeder-fuenfte-Patient-mit-seiner-Knie endoprothese-nicht-zufrieden (17.11.2017) · [5] Wang et al. 2015, Osteoarthritis and Cartilage 23, 22–30 · [6] Temiz Artmann et al. 2005, Methods and Findings in Experimental and Clinical Pharmacology, 27(6),391–394 · [7] Melzer et al. 2003, Fachkrankenhaus für Orthopädie · [8] Steinecker-Frohnwieser et al. 2014, Journal of Orthopedics and Rheumatology 9/2014 · [9] Kullich/Melzer 2019, Scientific evaluation of the MBST Magnetic Resonance Technology regarding the therapeutic potential and proof of clinical efficacy


MBST therapy for osteoarthritis · Overview