Guide Wound Healing · Acute and chronic wounds
A healthy organism is able to close wounds, i.e. defects in tissue, by its healing ability. However, more and more people nowadays suffer from chronic wounds that do not heal. Not only do chronic wounds usually cause severe pain, the risk of infection can increase, leading to disabilities in everyday actvities that massively restrict normal life.
Wound healing disorders
What to do if wound healing is problematic?
Wounds · Basic knowledge
A wound is a tissue injury (lesion) that results from a deep cut or superficial damage to the skin and mucous membranes, i.e. body cells are destroyed or die. Determining the cause of a wound is important for its assessment, as are the size, depth and the type of wound. The wound environment is another factor involved, whether there are signs of wound infection and wound pain. The consequences of a wound can be a loss of blood, some of which can be severe, and a loss of the protective function of the skin tissue, so that pathogens or foreign substances can enter the body and cause further damage.
Wounds can occur due to mechanical, thermal, chemical or radiation influences. Surgical wounds occur in the course of ambulatory department or residential invasive surgery of the body. Wounds disturb the function of the tissue and lead to a lower oxygen supply and blood circulation than in undamaged skin areas, whereby the healing process is slower.
The most common wound types (vulnus) are:
Wounds are categorised according to their time of origin: Until up to eight hours after tearing of the skin, wounds or injuries are defined as acute, fresh wounds. If the skin was torn more than eight hours ago, the expert speaks of an "old" wound. If a wound shows no improvement after four weeks or if the healing process of the wound without treatment takes more than eight weeks, it is called a "chronic" wound.
Wound healing · Complex biochemical processes
Wound healing involves complex biological processes that are vital for all organisms. In the healthy body, these natural processes usually take place without the need for medical measures. It is important that all non-surgical wounds have to be considered as infected and that the pathogens and damaged or inanimate tissue are removed. The earlier the patient is treated, the lower the risk of infection. It is also important to determine whether the patient suffers from primary diseases that might influence the process of wound healing, such as diabetes or tumours.
The wound healing process starts immediately after the injury. Cell debris or necrotic tissue are removed by macrophages. These in turn stimulate fibroblast production, which release collagen to close the wound. The following dynamic processes overlap in time and cannot be clearly separated. These normal wound healing processes include:

Acute wounds · Primary wound healing
An acute wound can happen quickly in everyday life. The term defines a new injury that disrupts the barrier the skin poses, for example cuts, abrasions, stab wounds, scratch wounds or minor burns. Acute wounds usually heal on their own within a short time and do not require any special treatment.
A doctor should be consulted if an acute wound is very deep, bleeding heavily, dirty or in case of all bite wounds. Uncomplicated healing of the wounds happens most easily when the margin of the wound are smooth and close, the body part affected has a good blood circulation and the wound area is free of foreign bodies or dead tissue.
If the wound is treated, sutured, clamped or glued, it can heal undisturbed and without complications within days to a few weeks under a dry, sterile bandage. In this case one speaks of primary wound healing.
Wound healing disorders · Causes
The healthy body tries to repair a wound as quickly as possible by forming new tissue to replace the destroyed one. In cases of wound healing disorders, the natural wound healing processes can be impeded or interrupted. If wound healing processes are not automatically triggered or disturbed, the consequences can be chronic pain, movement restrictions or even permanent nerve damage.
Usually, the biological processes of wound healing work smoothly, but it becomes problematic when they are impaired. If a wound has still not fully healed after six weeks, i.e. the wound heals very slowly or not at all, it is categorised as a chronic wound.
When time does not heal all wounds
If wound healing is affected negatively because there is no sufficient blood circulation in the wound area so that the margins of the wound mortifies or the wound breaks open again, germs and bacteria (pus and rot pathogens) can enter the wound and cause a wound healing disorder that may become chronic.
Disorders of the wound healing processes can be:
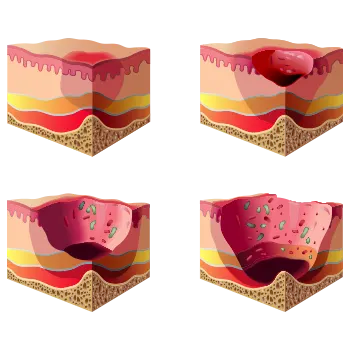
Chronic wounds · Missing tendency to heal
If a wound shows no signs of healing after four to twelve weeks despite professional care, it is already considered as chronic. If it is caused by circulatory disorders, as is the case with venous leg ulcers (ulcus cruris), the wounds can even go through several layers of skin down to the bones.
Scars · Hypertrophic scars
The process of scar formation is the end of wound healing. If a skin wound is closed again with connective tissue, a more or less large or conspicuous scar shows. Scars can be a cosmetic problem for the person affected, especially if they are bulging and stand out in colour. They may also lead to functional restrictions if the scar is situated at an inconvenient location, e. g. on a joint, or hard scar tissue develops.
A bulging scar that rises significantly above the skin level is caused by an overproduction of connective tissue fibres.
Diabetic foot
The so-called diabetic foot affects primarily patients with long-term and poorly managed diabetes. Nerves and blood vessels in the feet have been damaged by the disease, which can disturb blood circulation and sensitivity. In addition, the patient is usually more susceptible to infection because the immune system is weakened. Then small injuries or pressure points can result in large wounds that heal poorly due to circulatory disorders.
Open leg (Ulcus cruris)
The therapy of often deep wounds, such as venous leg ulcers, usually takes time while it is attempted to improve the disturbed blood circulation. The wound must be cleaned regularly to prevent infection.
Bed sores · Decubitus
Bed sores are caused by lasting pressure on an area of skin. Being bedridden in old age is a particular risk factor. The lack of blood circulation leads to skin and tissue damage in different stages. Such pressure ulcers can cause severe pain and can even be life-threatening. The therapy is often lengthy.
Wound pain · Danger of infection
A common symptom of chronic wounds is severe wound pain. The necessary treatment is also often painful. Due to the missing skin barrier, the risk of infection is high. As a result, the non-healing wounds can severely impede everyday life and massively reduce the quality of life.
MBST in the treatment of wound healing disorders
Molecular biophysical stimulation
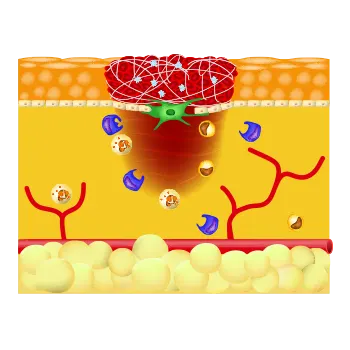
MBST therapy is based on the physical principle of magnetic resonance, in which hydrogen nuclei take up energy and then release it again partly into the surrounding tissue. Scientific data suggests that MBST magnetic resonance technology has an effect on connective tissue cells and the basic tissue formed by intercellular substance (ECM). It could be shown that several biophysical processes can be stimulated and that anti-inflammatory and pain-relieving effects can be triggered.[1–10] Damaged cells shall be influenced in such a way that natural regenerative processes can be triggered. The aim of MBST magnetic resonance therapy is to actively influence disturbed wound healing processes and effectively support the healing rates of chronic wounds.
MBST therapy has been shown to have significant success in the treatment of wound healing disorders and can support the healing of chronic wounds. Therapy aim is to repair tissue defects as quickly as possible, thus restoring the protective function of the skin and also to positively influence scar formation.
Internal clock influences wound healing
New research results in molecular and cell biology have increased our understanding of postsurgical care and physiological wound healing. Depending on the time of day when the injury or the invasive procedure occurred, a skin wound heals up to two times faster because, for example, the production of actin as well as the mobility of fibroblasts vary with the rhythm of the day.[11] The fibroblasts form a new extracellular matrix. The formed capillaries supply the tissue with the oxygen that the metabolism needs. Primary blood clots are broken down by agents of the fibrinolysis system: u-PA (urokinase plasminogen activator) and t-PA (tissue plasminogen activator). The various matrix metalloproteinases (MMP) also transform the extracellular matrix.[12]
The circadian cell rhythm influences the immigration of cells into the injured tissue and the formation of solid cell contacts.[11] The new findings may be of help to patients after surgery because the accelerated reaction can be helpful for the wound healing. Body cells that are out of sync or misregulated can no longer fulfill important processes, which can trigger, among other things, misregulations of the metabolism and disturbances in the interactions of molecular mechanisms. Tissue degeneration, disturbed regeneration processes and associated inflammatory reactions may follow.
Scientific data show that MBST technology can actively influence the internal clocks of cells, that are also important in wound healing [2,11]. Among other things, the aim is to reprogram these clocks in order to enable smooth running again. .
Postsurgical therapy approach
MBST therapy is used postsurgically to remedy tissue defects as quickly as possible, to restore the skin’s natural protective function and to positively influence scars. Aim of all postsurgical MBST wound treatment is a functionally stressable and aesthetically inconspicuous scar. A resilient scar is the best protection for the tissue against renewed opening or infections.
The development of pain following surgery is closely dependent on the exact procedure of incisions into the skin and the displacement of tissue such as bones or bone fragments. In this case, the surrounding tissue may be severely affected, which can result in postsurgical pain. Postsurgical pain is not only very unpleasant for the patient, but can also have an adverse effect on the respective healing process and prevent normal wound healing. This is where MBST magnetic resonance therapy comes in. Its aim is to influence wound healing processes, among other things, and also to reduce pain and inflammatory reactions by means of a targeted energy transfer into injured or dysfunctional tissue.
The advantages of MBST magnetic resonance therapy in the treatment of wound healing disorders at a glance:
[1] Steinecker-Frohnwieser et al. 2014, J Orthopedics Rheumatology, 9/2014 · [2] Egg et al. 2017 · [3] Digel et al. 2007, Med Bio Eng Comput, 45, 91–97 · [4] Artmann 2006 · [5] Artmann 2007 · [6] Oliva 2014 · [7] Kullich et al. 2013, SCHMERZ nachrichten 4a · [8] van Laack et al. 2011, Orthopädische Praxis 47, 11/2011, 536–543 · [9] Steinecker-Frohnwieser et al. 2009, Bone 44, 295, doi: 10.1016/j.bone.2009.03.537 · [10] Steinecker-Frohnwieser et al. 2017, Clinical and Experimental Rheumatology, PMID 29185963 · [11] Hoyle et al. 2017, Science Translational Medicine 9 (415), doi: https://doi.org/10.1126/scitranslmed.aal2774 · [12] Baker 2002, J Cell Sci 115, 3719–3727 · [13] Kullich/Melzer 2018, Scientific evaluation of the MBST Magnetic Resonance Technology regarding the therapeutic potential and proof of clinical efficacy


Detailed information about postsurgical MBST therapy